Introduction
Bruton's tyrosine kinase (BTK) inhibitors have proved to be a valuable treatment option for several B-cell malignancies, transforming outcomes for many patients.
In this short overview, hematologist Alessandra Tedeschi and pharmacologist Federico Pea outline the key pharmacotherapy considerations in the use of the BTK inhibitors ibrutinib, zanubrutinib, and acalabrutinib. Potential drug–drug interactions (DDIs) with BTK inhibitors and commonly prescribed medication are described, along with some background on mechanisms of DDIs.

Alessandra Tedeschi

Federico
Pea
BTK inhibition
Ibrutinib was the first-in-class BTK inhibitor, initially receiving approval for MCL in 2013.1 It offers deep and durable responses with an acceptable toxicity profile, but patients may experience side effects attributed to significant off-target activity.2 Cardiovascular adverse drug reactions are a notable challenge, with substantial real-world incidence of atrial fibrillation and hypertension among patients treated with ibrutinib.2-4
The next-generation BTK inhibitors zanubrutinib and acalabrutinib have greater selectivity for BTK compared with ibrutinib and have consistently demonstrated some notable advantages in terms of safety in head-to-head trials versus ibrutinib.5-7 Notably, zanubrutinib and acalabrutinib have favorable cardiac safety profiles compared with ibrutinib.5-7
Efficacy outcomes have usually been similar between BTK inhibitors in head-to-head trials. However, in the ALPINE study in relapsed/refractory (R/R) CLL, zanubrutinib demonstrated a better overall response rate (83.5% vs. 74.2%) and 24-month progression-free survival (78.4% vs. 65.9%; hazard ratio: 0.65; P=0.002) versus ibrutinib.7
These three covalent BTK inhibitors are currently approved as monotherapies by the European Medicines Agency (EMA) and the US Food and Drug Administration (FDA) for the treatment of four B-cell malignancies (see Table 1).8–13
Table 1. BTK inhibitor approvals in B-cell malignancies and pharmacology8–14
|
Ibrutinib |
Zanubrutinib |
Acalabrutinib |
|
| Approved indications in Europe (EMA) | CLL*, MCL, WM† | CLL, MZL, WM | CLL‡ |
| Approved indications in the USA (FDA) | CLL*, WM† | CLL, MCL, MZL, WM | CLL‡, MCL |
| Pharmaceutical forms in Europe (EMA) | Hard capsule: 140 mg Tablets: 140 mg, 280 mg, 420 mg, and 560 mg |
Hard capsule: 80 mg | Hard capsule: 100 mg Tablet: 100 mg |
| Pharmaceutical forms in the USA (FDA) | Capsules: 70 mg and 140 mg Tablets: 140 mg, 280 mg, and 420 mg Oral suspension: 70 mg/mL |
Hard capsule: 80 mg | Hard capsule: 100 mg Tablet: 100 mg |
| Approved dose | 420 mg QD for CLL and WM 560 mg QD for MCL |
160 mg BID or 320 mg QD | 100 mg BID |
| IC50 against BTK, nM | 1.5 | 0.5 | 5.1 |
| Potency of major active metabolite against BTK | ~15-fold less potent compared with the parent molecule | N/A | ~2-fold less potent compared with the parent molecule |
| Half-life, hours | ~4 to 6 | ~2 to 4 | ~0.6 to 2.8 |
| Plasma protein binding, % | 97.3–97.7 | ~94 | 97.4–97.5 |
| AUC0–24h (CV%), ng·h/mL | 420 mg QD: 707–1,159 (50%–72%) 560 mg QD: 865–978 (69%–82%) |
160 mg BID: 2,295 (37%) 320 mg QD: 2,180 (41%) |
100 mg BID: 1,843–1,850 (38%–72%) |
| fu. AUC0–24h, nM·h | 420 mg QD: 37–60 560 mg QD: 46–51 |
160 mg BID: 278 320 mg QD: 267 |
100 mg BID: 103 |
| Plasma exposure of major active metabolite | 1- to 2.8-fold higher than parent AUC | N/A | 2- to 3-fold higher than parent AUC |
| Median BTK occupancy in PBMC at trough | 420 mg to 820 mg QD: >90% | 160 mg BID: 100% 320 mg QD:100% |
100 mg BID: ≥95% |
| Median BTK occupancy in lymph node at trough | 420 mg QD: >90% | 160 mg BID: 100% 320 mg QD: 94% |
100 mg BID: 95.8% 200 mg QD: 90% |
| P-gp and brain penetration | Not a P-gp substrate. Brain penetration data in patients available. | Weak P-gp substrate. Brain penetration data in patients available. | P-gp substrate. Likely limited brain penetration. |
*Approved as monotherapy or with obinutuzumab, rituximab, or venetoclax for previously untreated CLL and as monotherapy or with bendamustine and rituximab for previously treated CLL. †Approved as monotherapy or with rituximab for previously treated patients and untreated patients unsuitable for chemoimmunotherapy. ‡Approved as monotherapy or with obinutuzumab. AUC, area under the curve; BID, twice a day; fu., fraction of unbound drug in plasma; IC50, half maximal inhibitory concentration; N/A, not applicable; PBMC, peripheral blood mononuclear cell; QD, once a day.
Tolerability with BTK inhibitors
Side effects associated with BTK inhibitors are usually manageable, but withdrawal or discontinuation of the agents may be required in some circumstances (see Table 2).2,5–7
Table 2. BTK inhibitor side effect management9,11,12
| Dose adjustments or discontinuation | |
| Ibrutinib |
|
| Zanubrutinib |
|
| Acalabrutinib |
|
DDI overview
Monitoring and managing the risk of potential DDIs is an important component of treatment with any drug, including BTK inhibitor therapy. Most patients with CLL, WM, MCL, or MZL are ≥60 years old at diagnosis and likely to have comorbidities that require medication.15–18 Acute conditions (such as infections) that require treatment will also arise over time in this patient population.
DDIs occur when one drug alters the activity of another drug and result from pharmacokinetic and/or pharmacodynamic mechanisms, both of which are relevant to BTK inhibitors (see Figure 1).19
Figure 1. DDIs with BTK inhibitors9,11,12,19,20
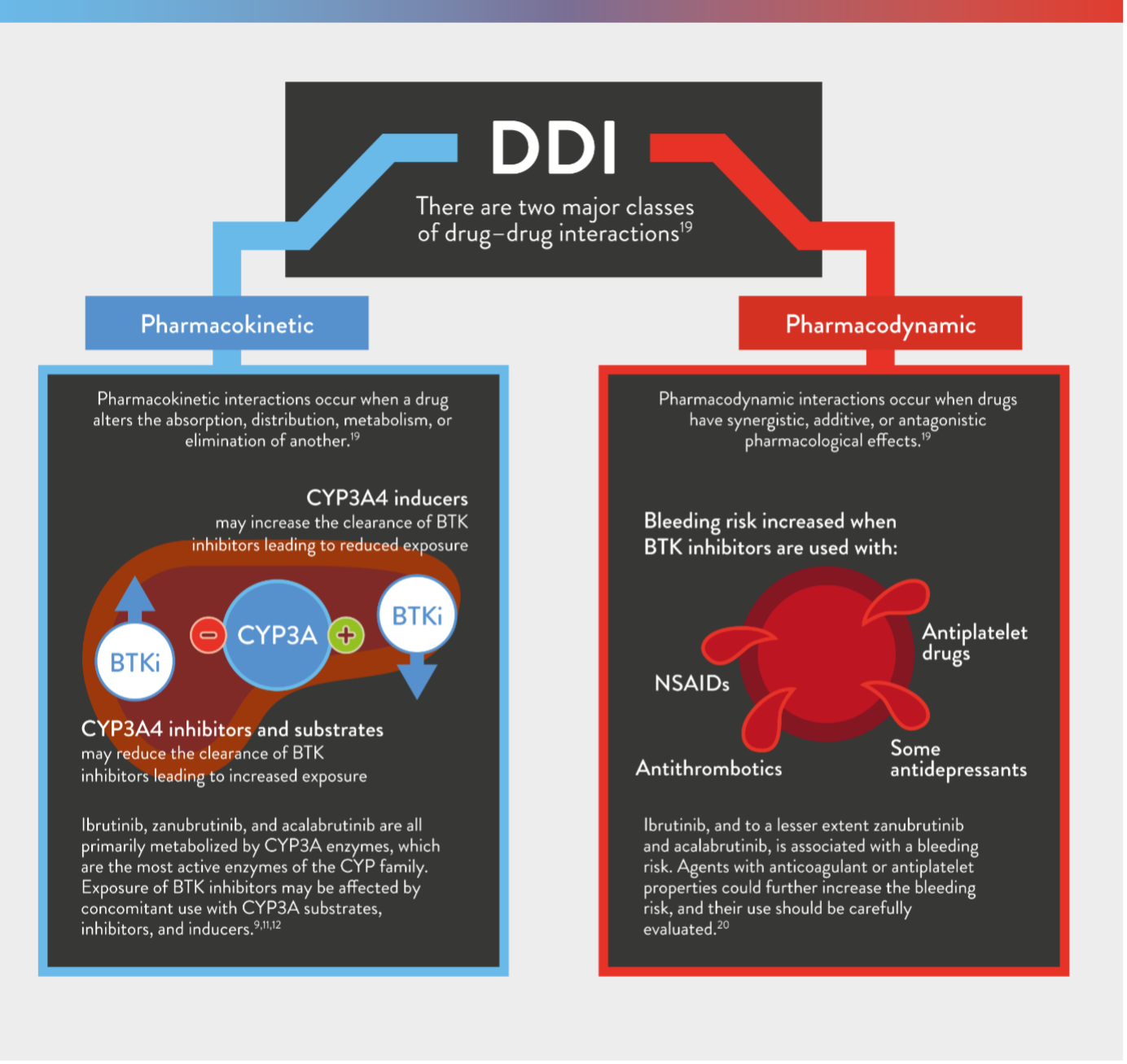
Table 3. Potential DDIs with ibrutinib, zanubrutinib, and acalabrutinib in patients with B-cell malignancies
Interaction strength: X major (highly clinically significant), ⚠ moderate (moderately clinically significant), and no known interaction. Interactions may increase (↑) or decrease (↓) a patient's exposure to a BTK inhibitor.| Alpha blockers | Analgesics | Angiotensin-II receptor blockers | Antibiotics | Anticholinergics | Anticonvulsants | Antidepressants | Antidiabetics | Antihistamines | Anti-emetics | Antifungals | Antiplatelet therapies | Antipsychotics | Antithrombotics | Beta blockers | Calcium channel blockers | Cardiac glycosides | Diuretics | Glucocorticoids | Hypnotics | Muscle relaxants | Non-steroidal anti-inflammatory drugs (NSAIDs) | Potassium channel blockers | Proton pump inhibitors (PPIs) | Sedatives | Statins | Urology | ||||||||||||||||||||||
| Tamsulosin, Terazosin | Acetaminophen, Buprenorphine, Celecoxib, Codeine, Fentanyl, Hydrocodone, Hydromorphone, Meperidine, Methadone, Oxycodone, Piroxicam, Tramadol | Irbesartan, Losartan, Valsartan | Clarithromycin | Clindamycin | Rifampin | Sulfamethoxazole | Benztropine | Carbamazepine | Ethosuximide | Phenytoin | Valproic acid | Amitriptyline | Bupropion | Citalopram | Duloxetine | Escitalopram | Fluoxetine | Mirtazapine | Paroxetine | Sertraline | Trazodone | Venlafaxine | Glipizide, Metformin, Pioglitazone, Rosiglitazone | Chlorpheniramine, Diphenhydramine, Hydroxyzine, Loratadine | Metoclopramide | Fluconazole | Isavuconazonium | Itraconazole | Voriconazole | Clopidogrel, Prasugrel, Ticagrelor | Aripiprazole, Haloperidol, Olanzapine, Risperidone, Quetiapine, Ziprasidone | Apixaban, Clopidogrel, Dabigatran, Rivaroxaban, Warfarin | Carvedilol, Metoprolol, Propranolol, Sotalol | Diltiazem | Felodipine | Verapamil | Digoxin | Triamterene | Fluticasone | Diazepam, Midazolam | Carisoprodol, Cyclobenzaprine, Tizanidine | Aspirin, Diclofenac, Etodolac, Ibuprofen, Indomethacin, Meloxicam, Naproxen, Piroxicam | Amiodarone | Esomeprazole, Lansoprazole, Omeprazole, Pantoprazole, Rabeprazole | Alprazolam, Diazepam, Eszopiclone, Zolpidem | Atorvastatin, Lovastatin, Rosuvastatin, Simvastatin | Sildenafil, Tadalafil | |
| Ibrutinib | Clarithromycin is a strong CYP3A4 inhibitorAvoid concomitant use | Rifampin is a strong CYP3A4 inducerAvoid concomitant use | Carbamazepine is a strong CYP3A4 inducerAvoid concomitant use | Phenytoin is a strong CYP3A4 inducerAvoid concomitant use | Citalopram may increase the risk of bleedingMonitor patients receiving concomitant medications associated with a bleeding risk for signs and symptoms of bleeding. | Duloxetine may increase the risk of bleedingMonitor patients receiving concomitant medications associated with a bleeding risk for signs and symptoms of bleeding. | Escitalopram may increase the risk of bleedingMonitor patients receiving concomitant medications associated with a bleeding risk for signs and symptoms of bleeding. | Fluoxetine may increase the risk of bleedingMonitor patients receiving concomitant medications associated with a bleeding risk for signs and symptoms of bleeding. | Paroxetine may increase the risk of bleedingMonitor patients receiving concomitant medications associated with a bleeding risk for signs and symptoms of bleeding. | Sertraline may increase the risk of bleedingMonitor patients receiving concomitant medications associated with a bleeding risk for signs and symptoms of bleeding. | Venlafaxine may increase the risk of bleedingMonitor patients receiving concomitant medications associated with a bleeding risk for signs and symptoms of bleeding. | Fluconazole is a strong CYP3A4 inhibitorAvoid concomitant use | Isavuconazonium is a strong CYP3A4 inhibitorAvoid concomitant use | Itraconazole is a strong CYP3A4 inhibitorAvoid concomitant use | Voriconazole is a strong CYP3A4 inhibitorAvoid concomitant use | Clopidogrel, prasugrel, and ticagrelor may increase the risk of bleedingMonitor patients receiving concomitant medications associated with a bleeding risk for signs and symptoms of bleeding. | Antithrombotics may increase the risk of bleeding Warfarin or other vitamin K antagonists should not be administered concomitantly with ibrutinib. Monitor patients receiving concomitant medications associated with a bleeding risk for signs and symptoms of bleeding. | Diltiazem is a moderate CYP3A4 inhibitorModify ibrutinib dose to 280 mg once daily | Verapamil is a moderate CYP3A4 inhibitorModify ibrutinib dose to 280 mg once daily | Digoxin is a P-gp substrateDigoxin should be taken at least 6 hours before or after ibrutinib. | NSAIDs may increase the risk of bleedingMonitor patients receiving concomitant medications associated with a bleeding risk for signs and symptoms of bleeding. | Amiodarone is a moderate CYP3A4 inhibitorModify ibrutinib dose to 280 mg once daily | ||||||||||||||||||||||||||
| Zanubrutinib | Clarithromycin is a strong CYP3A4 inhibitorModify zanubrutinib dose to 80 mg once daily | Rifampin is a strong CYP3A4 inducerAvoid concomitant use | Carbamazepine is a strong CYP3A4 inducerAvoid concomitant use | Phenytoin is a strong CYP3A4 inducerAvoid concomitant use | Citalopram may increase the risk of bleedingMonitor patients receiving concomitant medications associated with a bleeding risk for signs and symptoms of bleeding and monitor complete blood counts. | Duloxetine may increase the risk of bleedingMonitor patients receiving concomitant medications associated with a bleeding risk for signs and symptoms of bleeding and monitor complete blood counts. | Escitalopram may increase the risk of bleedingMonitor patients receiving concomitant medications associated with a bleeding risk for signs and symptoms of bleeding and monitor complete blood counts. | Fluoxetine may increase the risk of bleedingMonitor patients receiving concomitant medications associated with a bleeding risk for signs and symptoms of bleeding and monitor complete blood counts. | Paroxetine may increase the risk of bleedingMonitor patients receiving concomitant medications associated with a bleeding risk for signs and symptoms of bleeding and monitor complete blood counts. | Sertraline may increase the risk of bleedingMonitor patients receiving concomitant medications associated with a bleeding risk for signs and symptoms of bleeding and monitor complete blood counts. | Venlafaxine may increase the risk of bleedingMonitor patients receiving concomitant medications associated with a bleeding risk for signs and symptoms of bleeding and monitor complete blood counts. | Fluconazole is a strong CYP3A4 inhibitorModify zanubrutinib dose to 80 mg once daily | Itraconazole is a strong CYP3A4 inhibitorAvoid concomitant use | Itraconazole is a strong CYP3A4 inhibitorModify zanubrutinib dose to 80 mg once daily | Voriconazole is a strong CYP3A4 inhibitorModify zanubrutinib dose to 80 mg once daily | Clopidogrel, prasugrel, and ticagrelor may increase the risk of bleedingMonitor patients receiving concomitant medications associated with a bleeding risk for signs and symptoms of bleeding and monitor complete blood counts. | Antithrombotics may increase the risk of bleedingWarfarin or other vitamin K antagonists should not be administered concomitantly with zanubrutinib. Monitor patients receiving concomitant medications associated with a bleeding risk for signs and symptoms of bleeding and monitor complete blood counts. | Diltiazem is a moderate CYP3A4 inhibitorModify zanubrutinib dose to 80 mg once daily | Verapamil is a moderate CYP3A4 inhibitorModify zanubrutinib dose to 80 mg once daily | Digoxin is a P-gp substrateZanubrutinib may increase the concentration of digoxin. | NSAIDs may increase the risk of bleedingMonitor patients receiving concomitant medications associated with a bleeding risk for signs and symptoms of bleeding and monitor complete blood counts. | Amiodarone is a moderate CYP3A4 inhibitorModify zanubrutinib dose to 80 mg once daily | ||||||||||||||||||||||||||
| Acalabrutinib | Clarithromycin is a strong CYP3A4 inhibitorAvoid concomitant use | Rifampin is a strong CYP3A4 inducerAvoid concomitant use | Carbamazepine is a strong CYP3A4 inducerAvoid concomitant use | Phenytoin is a strong CYP3A4 inducerAvoid concomitant use | Citalopram may increase the risk of bleedingMonitor patients receiving concomitant medications associated with a bleeding risk for signs and symptoms of bleeding. | Duloxetine may increase the risk of bleedingMonitor patients receiving concomitant medications associated with a bleeding risk for signs and symptoms of bleeding. | Escitalopram may increase the risk of bleedingMonitor patients receiving concomitant medications associated with a bleeding risk for signs and symptoms of bleeding. | Fluoxetine may increase the risk of bleedingMonitor patients receiving concomitant medications associated with a bleeding risk for signs and symptoms of bleeding. | Paroxetine may increase the risk of bleedingMonitor patients receiving concomitant medications associated with a bleeding risk for signs and symptoms of bleeding. | Sertraline may increase the risk of bleedingMonitor patients receiving concomitant medications associated with a bleeding risk for signs and symptoms of bleeding. | Venlafaxine may increase the risk of bleedingMonitor patients receiving concomitant medications associated with a bleeding risk for signs and symptoms of bleeding. | Fluconazole is a strong CYP3A4 inhibitorAvoid concomitant use. | Itraconazole is a strong CYP3A4 inhibitorAvoid concomitant use | Itraconazole is a strong CYP3A4 inhibitorAvoid concomitant use. | Voriconazole is a strong CYP3A4 inhibitorAvoid concomitant use. | Clopidogrel, prasugrel, and ticagrelor may increase the risk of bleedingMonitor patients receiving concomitant medications associated with a bleeding risk for signs and symptoms of bleeding. | Antithrombotics may increase the risk of bleedingWarfarin or other vitamin K antagonists should not be administered concomitantly with acalabrutinib. Monitor patients receiving concomitant medications associated with a bleeding risk for signs and symptoms of bleeding. | Diltiazem is a moderate CYP3A4 inhibitorNo dose adjustment. Monitor patients closely for adverse reactions. | Verapamil is a moderate CYP3A4 inhibitorNo dose adjustment. Monitor patients closely for adverse reactions. | NSAIDs may increase the risk of bleedingMonitor patients receiving concomitant medications associated with a bleeding risk for signs and symptoms of bleeding. | Amiodarone is a moderate CYP3A4 inhibitorNo dose adjustment. Monitor patients closely for adverse reactions. | PPIs may interfere with acalabrutinib when administered as capsulesAvoid concomitant use with acalabrutinib 100 mg hard capsules; PPIs may be taken without dose adjustments with acalabrutinib 100 mg tablets. | ||||||||||||||||||||||||||
Key takeaway messages
- BTK inhibition has transformed outcomes for many patients with B-cell malignancies, but there are specific pharmacotherapy challenges associated with agents that are usually administered as continuous daily therapy, often over many years
- Covalent BTK inhibitors have the same mode of action, but next-generation agents have favorable safety profiles versus ibrutinib, with acalabrutinib (ELEVATE-RR) and zanubrutinib (ALPINE and ASPEN) leading to fewer treatment discontinuations and cardiovascular adverse events compared to ibrutinib
- Zanubrutinib has demonstrated superior efficacy versus ibrutinib in R/R CLL, while acalabrutinib showed non-inferior efficacy compared to ibrutinib
- Side effects associated with BTK inhibitors are usually manageable, but dose reductions or discontinuations are necessary in some circumstances
- At initial treatment selection and in the long-term management of patients, physicians must be aware of the potential for DDIs with BTK inhibitors
- Most of the clinically relevant DDIs with BTK inhibitors relate to concomitant usage with inhibitors or inducers of CYP3A4 and/or agents associated with a bleeding risk
Please refer to the current health authority-approved product information for definitive guidance on each medicine’s drug interactions and recommended management.8–13
References
- Drugs.com. Imbruvica FDA approval history. Available at: https://www.drugs.com/history/imbruvica.html. Accessed June 2023.
- Buske C, Jurczak W, Salem J-E et al. Managing Waldenström's macroglobulinemia with BTK inhibitors. Leukemia 2023; 37 (1): 35–46.
- Baptiste F, Cautela J, Ancedy Y et al. High incidence of atrial fibrillation in patients treated with ibrutinib. Open Heart 2019; 6 (1): e001049.
- Dickerson T, Wiczer T, Waller A et al. Hypertension and incident cardiovascular events following ibrutinib initiation. Blood 2019; 134 (22): 1919–1928.
- Byrd JC, Hillmen P, Ghia P et al. Acalabrutinib versus ibrutinib in previously treated chronic lymphocytic leukemia: Results of the first randomized phase III trial. J Clin Oncol 2021; 39 (31): 3441–3452.
- Tam CS, Opat S, D'Sa S et al. A randomized phase 3 trial of zanubrutinib vs ibrutinib in symptomatic Waldenström macroglobulinemia: The ASPEN study. Blood 2020; 136 (18): 2038–2050.
- Brown JR, Eichhorst B, Hillmen P et al. Zanubrutinib or ibrutinib in relapsed or refractory chronic lymphocytic leukemia. N Engl J Med 2023; 388 (4): 319–332.
- Pharmacyclics LLC. IMBRUVICA – US prescribing information. Pharmacyclics LLC; South San Francisco, CA, USA, May 2023.
- AstraZeneca AB. Calquence 100 mg hard capsules – summary of product characteristics. AstraZeneca AB; Södertälje, Sweden, May 2023.
- AstraZeneca Pharmaceuticals LP. CALQUENCE (acalabrutinib) tablets, for oral use – US prescribing information. AstraZeneca Pharmaceuticals LP; Wilmington, DE, USA, August 2022.
- Janssen-Cilag International NV. IMBRUVICA 140 mg hard capsules – summary of product characteristics. Janssen-Cilag International NV; Beerse, Belgium, April 2023.
- BeiGene Ireland Ltd. BRUKINSA 80 mg hard capsules – summary of product characteristics. BeiGene Ireland Ltd; Dublin, Ireland, March 2023.
- BeiGene USA, Inc. BRUKINSA (zanubrutinib) capsules, for oral use – US prescribing information. BeiGene USA, Inc., San Mateo, CA, USA, April 2023.
- Tam CS, Ou YC, Trotman J et al. Clinical pharmacology and PK/PD translation of the second-generation Bruton's tyrosine kinase inhibitor, zanubrutinib. Expert Rev Clin Pharmacol 2021; 14 (11): 1329–1344.
- Eichhorst B, Robak T, Montserrat E et al. Chronic lymphocytic leukaemia: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 2021; 32 (1): 23–33.
- Dreyling M, Campo E, Hermine O et al. Newly diagnosed and relapsed mantle cell lymphoma: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 2017; 28 (Suppl 4): iv62–iv71.
- Cheah CY, Zucca E, Rossi D et al. Marginal zone lymphoma: Present status and future perspectives. Haematologica 2022; 107 (1): 35–43.
- Kastritis E, Leblond V, Dimopoulos MA et al. Waldenström's macroglobulinaemia: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 2018; 29 (Suppl 4): iv41–iv50.
- Niu J, Straubinger RM and Mager DE. Pharmacodynamic drug–drug interactions. Clin Pharmacol Ther 2019; 105 (6): 1395–1406.
- Fancher KM and Pappacena JJ. Drug interactions with Bruton's tyrosine kinase inhibitors: Clinical implications and management. Cancer Chemother Pharmacol 2020; 86 (4): 507–515.
- de Abajo FJ, García-Rodríguez LA. Risk of upper gastrointestinal tract bleeding associated with selective serotonin reuptake inhibitors and venlafaxine therapy: interaction with nonsteroidal anti-inflammatory drugs and effect of acid-suppressing agents. Arch Gen Psychiatry 2008; 65 (7): 795–803.
- Pilla Reddy V, Fretland AJ, Zhou D et al. Mechanistic physiology-based pharmacokinetic modeling to elucidate vincristine-induced peripheral neuropathy following treatment with novel kinase inhibitors. Cancer Chemother Pharmacol 2021; 88 (3): 451–464.